April 30, 2021
While COVID-19 upended most people’s lives for more than a year, the motivation to adapt and change behavior was rooted in the belief that there would be an eventual return to pre-COVID normalcy. As rising hospitalizations and lives lost dominated daily headlines, it was difficult to ignore the disproportionate impact of this disease on disadvantaged communities in the U.S. Although the prevalence of underlying health issues in certain populations contributed to the high mortality rate, some of the communities hardest hit by COVID-19 were plagued by a variety of causal factors.
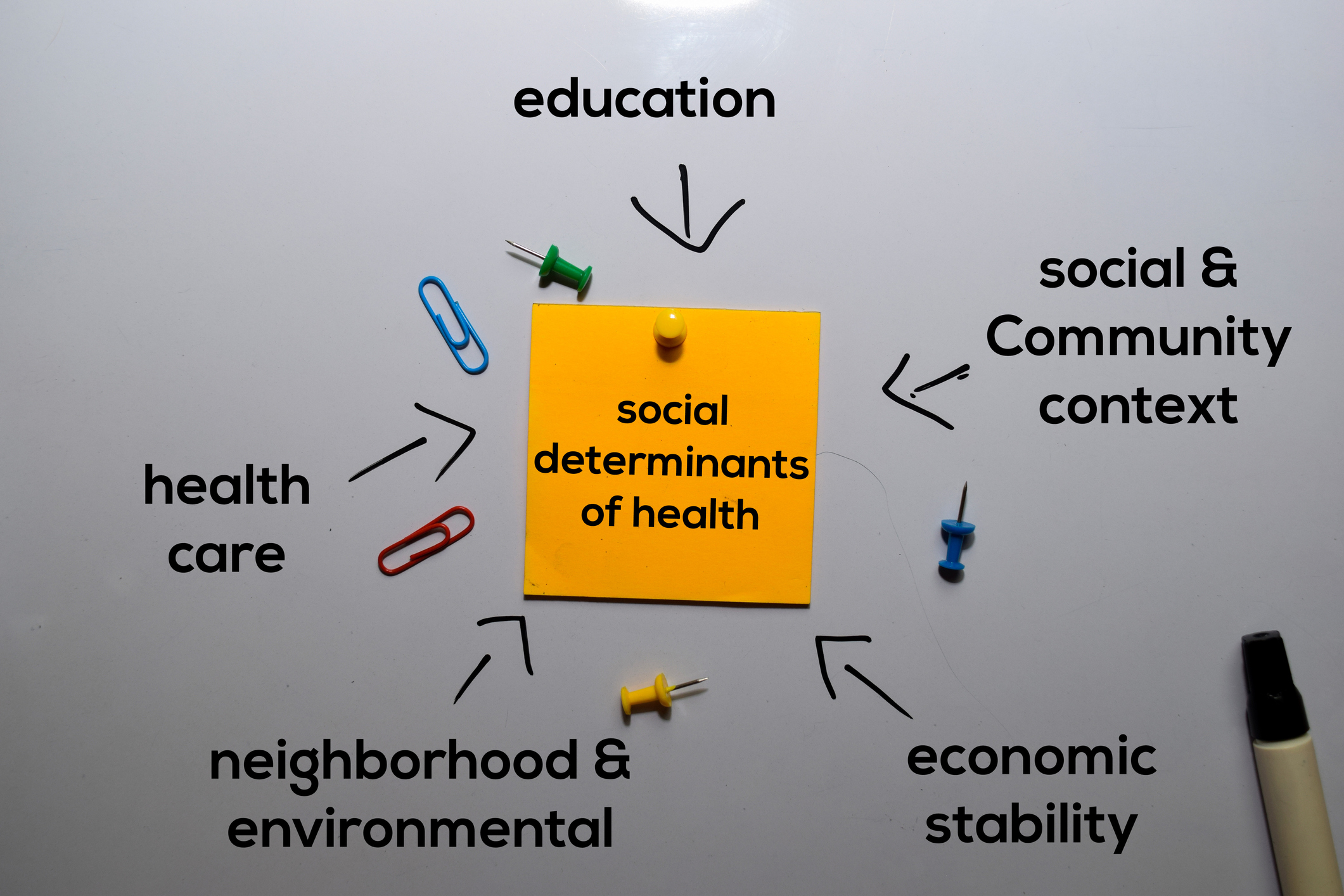
Public health experts initially focused on and attributed the high hospitalization and death rate among black, brown, and indigenous communities to risk factors like obesity, hypertension, chronic lung disease, and diabetes. But in addition to pre-existing medical conditions, there were other root causes. The health of an individual or an entire community is not based solely on direct clinical encounters. A person’s social, economic, and physical environment, the social determinants of health, influence outcomes more than any other factors.
We recognized that many low wage-earning frontline workers could not take time off even when symptomatic, putting other people at risk. Those living in densely populated urban areas often resided in multigenerational households due to cultural preferences or out of economic necessity. They were more likely to contract the virus because of unavoidable person-to-person interaction and reliance on public transportation. Work from home was not an option for most essential workers.
Conversations about systemic inequities are always complicated, but a return to “normal” without advancing a plan for future health equity leaves us all more vulnerable to the next deadly virus. A more destructive pandemic could change the trajectory of life as we know it if we are unprepared. Will limited access to preventative health care, reliance on overburdened, underfunded safety-net hospitals in heavily populated communities be part of returning to normal? With every catastrophe, there is the opportunity for change, a time to leverage lessons learned and work toward creating the infrastructure needed to bring health equity to marginalized communities. As employers, becoming more familiar with the concept and educating those around us is an excellent first step.
A couple of brief insightful videos:
Yale School of Medicine: Understanding COVID-19: Health Equity
Kaiser Permanente: Pandemic Highlights Urgent Need for Equity in Health Care
Please feel free to contact us at 312-648-1565 if you have any questions or concerns.
